How To Treat Diverticulitis Effectively

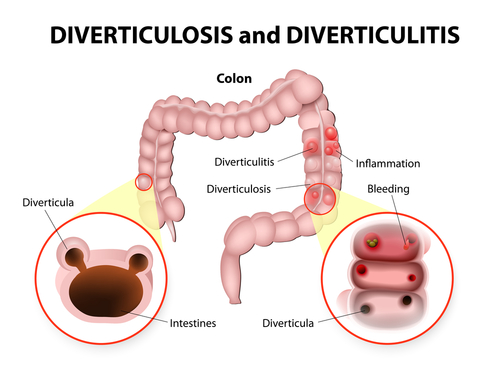
Diverticulitis (die-vur-tik-yoo-LIE-tis) is a condition that occurs when small pouches, called diverticula, form in the digestive tract and become inflamed or infected. Diverticula usually form in the colon as we age. The colon is the part of the large intestine that is responsible for removing waste from the body. As we age, the muscle in the wall of the colon can become weaker and weaker. When too much pressure, either from hard stools or straining during bowel movements, is placed on the weakened colon wall, the pouches can bulge out. This is called diverticulosis. Diverticulosis is very common. Over 50 percent of people older than age 60 have diverticula in their digestive tract and up to 2.5 million people in the US have diverticular disease.
 In many patients, diverticulosis does not cause any symptoms and does not require any treatment. Recently, experts have determined that many more patients have symptoms than we previously thought. This has spawned some interesting new disease names. Some patients with diverticulosis have a condition call SUDD (symptomatic uncomplicated diverticular disease) with symptoms of vague abdominal pain, bloating and altered bowel habit, similar to irritable bowel syndrome. A smaller number of patients will develop a condition called SCAD (segmental colitis associated with diverticulosis) or diverticular colitis, with symptoms of crampy pain and bloody diarrhea, similar ulcerative colitis or Crohn’s disease.
In many patients, diverticulosis does not cause any symptoms and does not require any treatment. Recently, experts have determined that many more patients have symptoms than we previously thought. This has spawned some interesting new disease names. Some patients with diverticulosis have a condition call SUDD (symptomatic uncomplicated diverticular disease) with symptoms of vague abdominal pain, bloating and altered bowel habit, similar to irritable bowel syndrome. A smaller number of patients will develop a condition called SCAD (segmental colitis associated with diverticulosis) or diverticular colitis, with symptoms of crampy pain and bloody diarrhea, similar ulcerative colitis or Crohn’s disease.
However, if the bulging pouches become infected, either from increased pressure in the colon or from a small tear or abrasion, diverticulitis may occur. Diverticulitis can feel similar to appendicitis except for the pain in diverticulitis is usually on the left side, not the right side. In addition to severe pain in the lower abdomen, many will suffer from bloating, fever, and nausea. Some patients will develop peritonitis from a perforation or abscess.
Diverticulitis can be acute or chronic. With chronic diverticulitis, the initial inflammation and infection may subside for a period of time, but it will never clear up completely. This could lead to bowel obstruction, causing constipation, diarrhea, abdominal swelling or bloating and constant abdominal pain. Acute diverticulitis appears as one or more severe attacks of infection that eventually go away for good. While we once thought that all patients with acute diverticulitis should receive antibiotics, it turns out that many patients will recover on their own.
Risk factors for diverticulitis include:
- Aging
- Diet high in animal fat and low in fiber
- Heredity
- Obesity
- Not enough physical activity
- Smoking
- Certain medications including steroids, opiates and nonsteroidal anti-inflammatory drugs, such as ibuprofen (Advil, Motrin IB, others) and naproxen (Aleve)
Symptoms of diverticulitis include:
- Severe abdominal pain
- Fever
- Nausea
- Abdominal tenderness
- A persistent change in bowel movements
In the past, we recommended a diet high in fiber and low in hard seeds and nuts to any patient with diverticulosis and a low residue diet for anyone recovering from diverticulitis. It turns out that the evidence for this is pretty low. There is no longer agreement that a high fiber diet really changes anything. And a large study recently showed that patients who consume corn, nuts or popcorn actually have fewer episodes of diverticulitis, not more. Still, many doctors will still make “old school” recommendations for management.
If you are experiencing any of the symptoms listed above, it is important to see a specialist. While mild diverticulitis can be treated with changes in your diet, extra rest and antibiotics, severe or recurring diverticulitis may require surgery. Our board-certified physicians at Greater Boston Gastroenterology will examine your abdomen, possibly do a blood test and/or CT scans, and then diagnose and plan a treatment method with you going forward. Treatment depends on the severity of your symptoms.
